The Technical Skills that Carry Weight Once You’re on the Floor

Everyone knows you need to master ICD-10-CM, CPT, and HCPCS. But did you know the 2026 CPT code set includes 418 total changes? They span digital health, AI-augmented services, cardiology, and vascular care.
Translation?
Static knowledge is dead knowledge.
The coders thriving in 2026 are the ones who've become comfortable with perpetual learning. They're actively tracking CMS updates, reading through the Journal of American Health Information Management Association (AHIMA), and frankly, treating code updates like some people treat fantasy football stats.
Insurance companies are getting ruthless about denials, and coders who understand how to link diagnosis codes to procedure codes in ways that clearly demonstrate medical necessity are worth their weight. One small misstep and that claim gets kicked back faster than you can say "revenue cycle management."
Then there's the EHR systems proficiency that goes beyond basic data entry. Epic, Cerner, and Meditech are platforms that have become coders' primary workspace. According to AHIMA, health information technology is a vital part of the coding process, and coders must be proficient in using HIT systems and software.
You need to understand how documentation flows through them, where physicians typically make documentation errors, and how to efficiently query incomplete records.
The Medical Coding Soft Skills Above the Rest
Technical chops will get you hired. Soft skills will get you promoted and keep you employed when automation inevitably comes knocking.
Communication skills top this list. Medical coders need to know how to diplomatically tell a physician that their documentation is garbage without saying those words. You're constantly bridging gaps between clinical staff who think in diagnoses and billing departments who think in dollar signs.
Analytical thinking is also critical for medical coding professionals, as the ability to analyze complex medical records, identify patterns, and interpret information is crucial for accurate coding. When you encounter incomplete or ambiguous documentation (which happens about 40% of the time in a typical hospital setting), you can't just guess. You need to piece together context clues from lab results, medication lists, and procedure notes to determine what probably happened, then confirm with the appropriate provider.
Adaptability deserves its own paragraph because 2026 is throwing curveballs monthly.
"Medical Coding adoption requires centralized information. Instead of visiting multiple platforms, coders should access everything they need in one place, boosting efficiency."
– June Bronnert, RHIA, CCS, CCS-P, Director of Professional Practice Resources at AHIMA
But this efficiency comes with a learning curve. Computer-assisted coding (CAC) systems and AI-driven platforms change workflows. The coders who panic at every new software rollout will get left behind. The ones who see each change as a tool to make their jobs easier? Those are your future coding managers.
The Stats that Match the Skills

- Employment of medical records specialists – including medical billers and coders – is expected to grow by 9% from 2023 to 2033, with 16,700 new jobs expected to be added over this period.
- Compare that to the national average job growth of 4%, and you're looking at a field with staying power.
- Not all medical coding jobs are created equal. The average salary sits around $53,690, but coders with specialty certifications are pulling in significantly more. Risk adjustment coders, DRG specialists, and auditors with the Certified Billing and Coding Specialist (CBCS) credential are commanding salaries at the higher end of the spectrum.
The Training Path that Elevates Your Medical Coding Skills
Where you get trained can dramatically impact how quickly you become ready to enter the market. Community colleges offer solid programs, but they typically take 1-2 years and cost between $2,000-$10,000 annually, before factoring in books and materials. Online colleges provide flexibility but often run $8,000-$19,000 per year.
Programs like Health Tech Academy have disrupted this model. 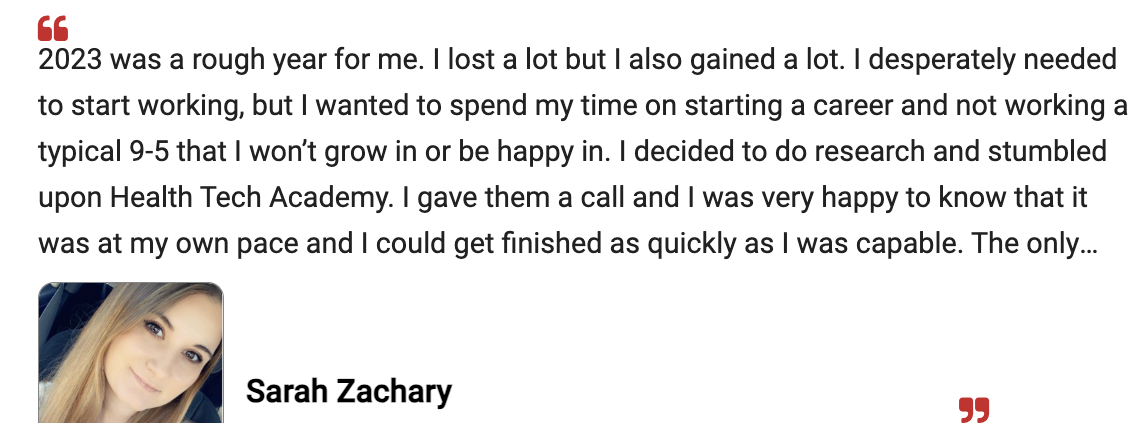
For a one-time cost of $2,500 (with books and certification exam fees included), students can enter the workforce within 4-6 months through a 100% online format with 1-on-1 coaching and job placement assistance.
Health Tech Academy vs Community and Online Colleges
| Feature | Health Tech Academy | Community College | Online Colleges |
|---|---|---|---|
| Program & Tuition Cost | $2,500 | $4,864 on average | $9,600+ |
| Books, Materials & Fees | Included | Additional $250-$500 | — |
| Certification Exams & Fees | Included | + $100 to $150 | + $100 to $150 |
| Job Ready In | 3-4 months | 1-2 years | 1-2 years |
| Clear Path to Certification | ✓ Yes | ✗ Sometimes | ✗ Sometimes |
| 1-on-1 Career Coaching | ✓ Yes | — | — |
| Schedule Flexibility | High | — | Varies |
| Travel Requirements | None | Required for in-person courses and labs | None |
| Content Delivery | All online | Varies | All online |
Before you formally take the exam, enroll and take our free Medical Coding practice exam.
The practice exam gives you an honest assessment of where you stand.
How AI and Automation Influence Medical Coding
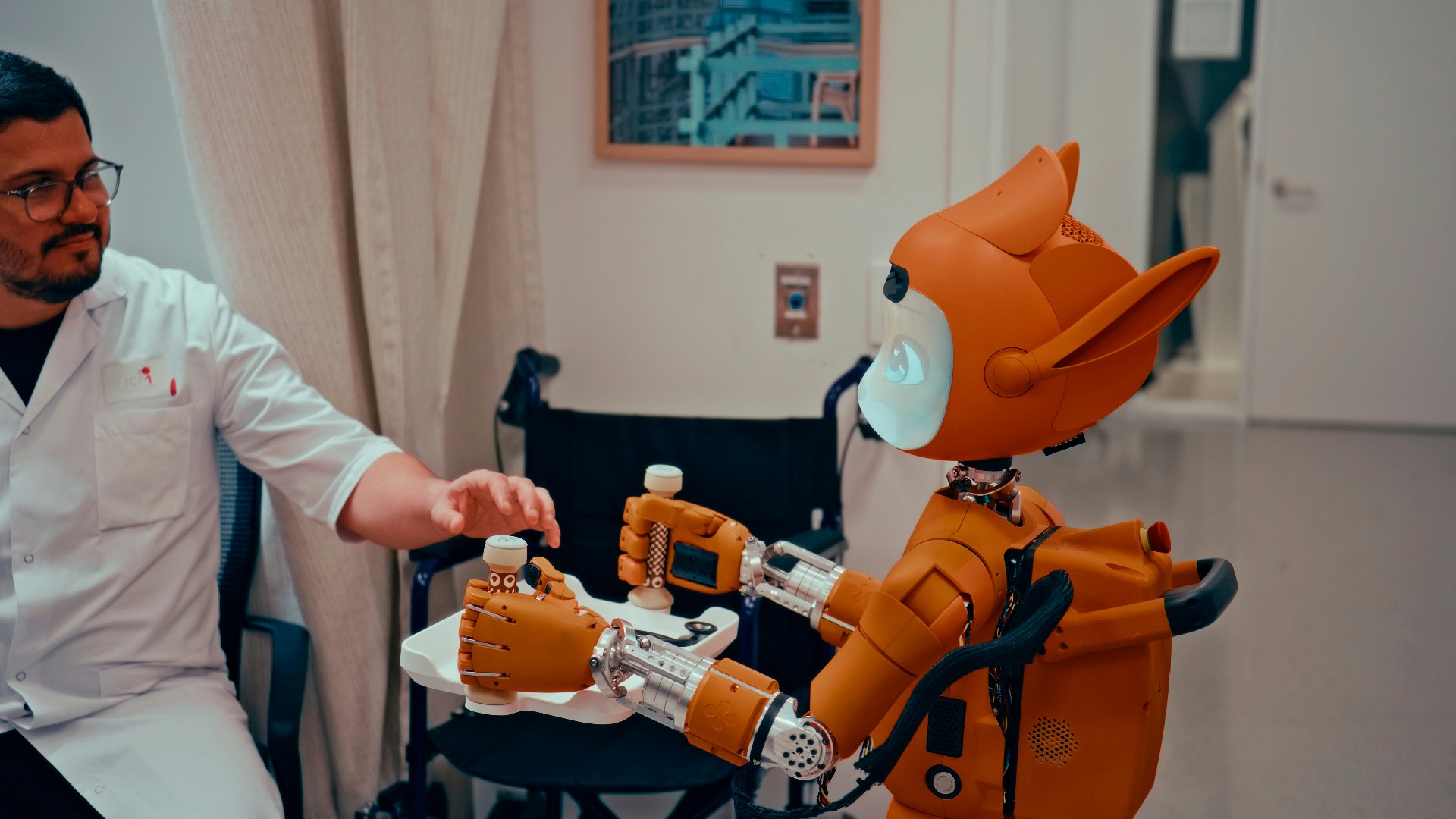
Yes, AI is coming for parts of medical coding. But it's not the job-ending apocalypse some people fear. The coders who will struggle are those who refuse to adapt.
"AI isn’t here to replace us. Coders will need to embrace lifelong learning and adapt to new tools."
– Mary Beth Haugen, RHIA, MS, Founder & CEO of Haugen Consulting Group
AI is an extremely fast but occasionally clueless assistant. It can suggest codes based on documentation patterns, but it can't understand clinical context the way a trained human can. A recent study found that even advanced AI coding systems require human oversight to catch errors that could lead to compliance issues or claim denials.
Your job is to become the expert who validates AI suggestions, catch its mistakes, and handles the complex cases that require genuine medical knowledge and critical thinking.
Watch and Listen to Our Podcast on Transforming the Healthcare Workforce Using AI
The Certification Question: CPC, CCS, or CBCS?

Both AAPC and AHIMA certifications are respected, but they serve slightly different purposes.
- AAPC's Certified Professional Coder (CPC) credential is great for outpatient coding.
- AHIMA's Certified Coding Specialist (CCS) leans toward inpatient hospital coding.
Then there's the National Health Career Association's CBCS, which covers both billing and coding competencies in a single credential. The CBCS is particularly valuable for entry-level professionals because it demonstrates dual expertise.
You’re translating diagnoses into codes and understanding how those codes move through the entire revenue cycle. For smaller medical practices that need someone who can wear both hats, the CBCS credential makes you immediately more hireable.
For 2026, the CPC has an edge for most entry-level coders simply because outpatient settings represent most available positions. Plus, the exam is slightly less expensive, and AAPC membership benefits include networking opportunities that can be genuinely useful for job hunting. The CBCS, however, is ideal if you want maximum career advancement flexibility.
What the Job is Like
Medical coding isn't glamorous. You're not going to have heartwarming moments with patients or perform life-saving procedures. You’ll have:
- Steady work.
- The ability to work remotely in pajamas.
- A schedule that doesn't involve nights and weekends (mostly).
- The satisfaction of knowing that your accuracy directly impacts whether healthcare facilities can keep their doors open.
A typical day involves reviewing medical documentation, assigning appropriate codes, querying physicians for clarification, and working through denied claims to understand what went wrong. You'll spend significant time in EHR systems, consulting coding manuals, and probably more time than you'd like on the phone with insurance companies.
Once you develop true expertise in a specialty, you become nearly irreplaceable. Facilities will compete for you. You'll have leverage to negotiate remote work, higher pay, and forgiving schedules. That's the long game, and it starts with building the right skill foundation now.
If you're serious about breaking into medical coding, the time to start is now. The job market is strong, but competition is increasing as more people discover this career path.
- Get trained efficiently.
- Earn your certification.
- Build a skill set that goes beyond the basics.
The healthcare system needs accurate, knowledgeable coders more than ever, so make sure you're one of them.
Frequently Asked Questions and Answers
- How Long does it Take to Become a Certified Medical Coder: It depends entirely on your training path and how much time you can dedicate. Intensive programs like Health Tech Academy can get you ready in 4-6 months. Traditional community college programs typically take 1-2 years. The certification exam itself takes 4-5 hours for AAPC's CPC exam, but you'll want several months of prep time before attempting it. Most successful coders spend 15-20 hours per week studying for at least 3-4 months.
- Can I Work from Home as a Medical Coder: Absolutely, but typically not right away. Most employers want you to have 1-2 years of experience before going fully remote, though some larger healthcare systems offer hybrid arrangements. Once you've proven your accuracy and productivity, remote opportunities are plentiful. Just be prepared for your home office to require HIPAA-compliant internet security and possibly VPN access.
- What's the Difference Between Medical Coding and Medical Billing: Medical coders translate diagnoses and procedures into standardized codes. Medical billers take those codes and create insurance claims, follow up on payments, and handle patient billing questions. They're related but distinct roles requiring different skill sets. Many smaller practices hire people to do both, which is why combined billing and coding training makes sense. If you had to pick one to specialize in, coding typically offers higher pay and more advancement opportunities.
- Will AI replace Medical Coders: AI will change medical coding, not eliminate it. Computer-assisted coding already exists. However, AI lacks the clinical judgment and contextual understanding that experienced coders bring to complex cases. The coders at risk are those doing straightforward, high-volume coding that AI can handle. The coders who will thrive are those who specialize, understand compliance issues, can audit AI-generated codes, and handle complicated cases requiring human expertise.
- Do I Need a College Degree to Become a Medical Coder: No, you don't need a traditional four-year degree. Most coders complete a specialized training program and earn an industry certification. Many companies will hire based solely on certification and demonstrated competency.