The healthcare revenue cycle needs professionals who speak the language of insurance companies. According to the Bureau of Labor Statistics, medical records specialists (which includes medical coders and billers) will see 8% job growth through 2032, adding approximately 15,000 new positions to the field. But the variety of career paths most people will never hear about until they're already in the industry.
The Entry Points Everyone Starts From
Fresh graduates typically become a medical billing specialist or medical coding specialist. These aren't interchangeable titles, despite what your cousin who "works in healthcare" might tell you at Thanksgiving.
- Medical billing specialists handle the money side. They submit claims to insurance companies, follow up on denials, and essentially make sure healthcare providers get paid for their work. Entry-level positions start around $38,000 annually, according to recent PayScale data, though that jumps significantly with experience and certifications.
- Medical coding specialists translate medical procedures and diagnoses into standardized codes. They are like healthcare translators who turn "patient presented with acute bronchitis" into alphanumeric codes that insurance companies recognize. Starting salaries hover around $42,000, per the AAPC's 2023 salary survey.
"The biggest misconception is that coding and billing are the same job. Coders must understand anatomy, medical terminology, and clinical documentation, while billers focus on insurance contracts, payment posting, and accounts receivable. They’re complementary skills – but very different wheelhouses."
– Michelle Dick, CPC, Healthcare Educator and former Coding Manager at a multi-specialty practice in Ohio
The Mid-Career Pivot Points

After two to three years, your career branches into specialties:
- Certified Professional Coder (CPC) positions focus on outpatient coding and can pull $52,000 to $65,000 depending on location. But specialize further, and you're looking at $60,000 to $75,000. The AAPC reports that coders with specialty credentials earn approximately 20% more than their generalist counterparts.
- Medical Auditors review coded charts for accuracy and compliance, catching errors before they become fraud investigations. These positions start around $58,000 and can reach $80,000+ with experience.
- Revenue Cycle Specialists manage the entire patient financial journey, from registration through final payment. Salaries range from $48,000 to $72,000, with the higher end reserved for those managing teams or handling complex payer contracts.
- Coding Educators and Compliance Officers represent the fork in the road for people who want out of production work. Educators train new coders and can earn $55,000 to $85,000. Compliance officers ensure healthcare organizations follow billing regulations – critical work that commands $65,000 to $95,000.
The Leadership Track for Medical Billing and Coding

Stick around long enough, prove you can manage both people and processes, and you'll earn titles that sound boring but pay exceptionally well.
- Health Information Management (HIM) Directors oversee entire coding and billing departments. Salaries start at $75,000 and stretch past $110,000 in major metropolitan areas or large health systems. These roles require understanding both the technical side of coding and the business side of healthcare finance.
- Revenue Cycle Directors sit even higher on the org chart, managing everything from patient access to final collections. We're talking $95,000 to $140,000+, depending on the organization's size.
According to HFMA's 2023 revenue cycle compensation survey, professionals with 10+ years of experience in revenue cycle leadership roles report median total compensation of $127,000 (and that's not counting bonuses tied to metrics like days in accounts receivable or clean claim rates).
"The career ladder in medical coding and billing rewards professionals who stay current with regulations and technology. As healthcare shifts toward value-based care, demand is growing for those who understand both coding and the analytics behind healthcare finance."
– Robert Tennant, MA, Senior Policy Advisor at MGMA
The Non-Traditional Paths You Could Explore
Major companies like Optum, 3M, and Humana regularly hire remote coders at competitive rates – $45,000 to $70,000 depending on specialty and experience. Some coders piece together contract work from multiple organizations, effectively freelancing their way to six figures while working from a coffee shop in Bali (though insurance compliance rules make this trickier than it sounds).
Consulting represents another off-ramp for experienced coders. Healthcare practices regularly hire consultants to audit their coding, optimize their revenue cycle, or train staff on new specialties. Hourly rates for coding consultants range from $50 to $150, depending on expertise and the complexity of the engagement.
The Medical Billing and Coding Certification Question

Certified coders earn 27% more than non-certified coders on average, per AAPC data.
- The Certified Professional Coder (CPC) and Certified Billing and Coding Specialist (CBCS) credentials are the industry standard for outpatient coding.
- The Certified Coding Specialist (CCS) credential from AHIMA carries weight for inpatient hospital coding.
- Specialty certifications in areas like interventional radiology (CIRC) or risk adjustment coding (CRC) add another salary bump.
Comparing Your Training Options
Before you drop serious money on a degree program, consider what you need to break into this field:
Health Tech Academy vs Community and Online Colleges
| Feature | Health Tech Academy | Community College | Online Colleges |
|---|---|---|---|
| Program & Tuition Cost | $2,500 | $4,864 on average | $9,600+ |
| Books, Materials, & Fees | Included | Additional $250-$500 | — |
| Certification Exams & Fees | Included | + $100 to $150 | + $100 to $150 |
| Job Ready In | 3-4 months | 1-2 years | 1-2 years |
| Clear Path to Certification | ✓ Yes | ✗ Sometimes | ✗ Sometimes |
| 1-on-1 Career Coaching | ✓ Yes | — | — |
| Schedule Flexibility | High | — | Varies |
| Travel Requirements | None | Required for in-person courses and labs | None |
| Content Delivery | All online | Varies | All online |
Most employers care about certification and experience, not where you went to school. A four-month focused program that includes exam prep gets you earning faster than a two-year associate degree that covers anatomy, psychology, and general education requirements you don't need for coding work.
Start your medical coding and billing career faster.
Health Tech Academy's program gets you certified and job-ready in 4-6 months – with exam fees included and 1-on-1 coaching throughout.
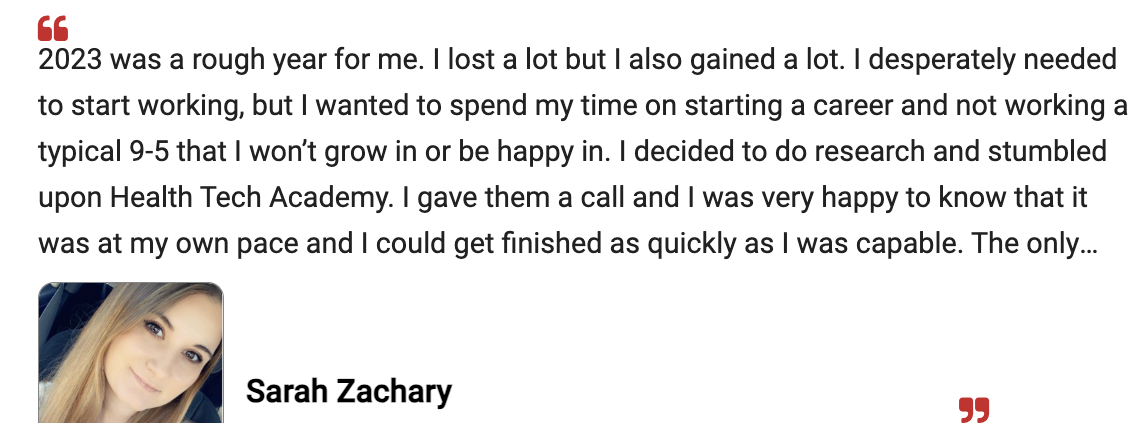
Hear From One of Our Students
The Bottom Line on Medical Billing and Coding Earnings Potential
A medical coder in rural Mississippi might start at $35,000, while the same position in San Francisco commands $58,000. But even accounting for cost of living, certain markets pay better. California, Massachusetts, New York, New Jersey, and Washington consistently top the salary charts for medical coding and billing positions.
Work setting matters too. Hospital-employed coders typically earn more than those in physician practices. Large health systems with union representation can offer compensation packages that top tech company benefits:
- Full healthcare.
- Pension plans.
- Generous PTO.
- Tuition reimbursement for continuing education.
Most choose to combine specialty certification, remote work flexibility, and contract opportunities.
Medical billing and coding is not going to make you wealthy overnight. But it offers a stable career with legitimate growth potential that doesn't require years of expensive schooling or mountains of student debt. In a healthcare industry that runs on accurate coding and timely reimbursement, these jobs aren't going anywhere, and the people who do them well will always be in demand.
Frequently Asked Questions and Answers
How Long Does It Take to Become a Certified Medical Coder?
Most focused certification programs take 4-6 months to complete if you're studying full-time, though some people stretch it to 9-12 months while working another job. After completing coursework, you'll sit for a certification exam. Community college associate degree programs take 1-2 years but include general education courses not directly related to coding.
Can You Work from Home as a Medical Biller or Coder?
Absolutely. Remote positions have become standard in this field. Many employers hire remote coders nationwide, though you'll typically need at least 1-2 years of experience first. Some organizations do hire entry-level remote positions, but they're more selective about candidates.
Do Medical Billers and Coders Need to Continue Their Education?
Yes. Maintaining certification requires continuing education units (CEUs) – typically 36 CEUs every two years for AAPC credentials. Medical coding changes constantly as new procedures emerge and regulations shift. Staying current is built into the certification requirements.
Is Medical Coding Being Replaced by Artificial Intelligence?
Not anytime soon. AI assists with coding by suggesting codes, but human coders still review for accuracy, handle complex cases, and ensure compliance. The role is evolving toward auditing AI suggestions and managing exception cases rather than coding every chart manually. This increases the need for highly skilled coders who understand both coding and technology.